“To err is human;to forgive,divine.”Remembering the famous poetry quote[1] by Alexander Pope (1688-1744).This means any human can make a mistake,so we should try to forgive them, just as,God said to show divine mercy to sinners and forgive them.Apart from medication error and faulty techniques, anaesthesiologists rarely make serious mistakes and any such mistake,if done may jeopardize the patient's life.It is usual that anaesthesiologists forget to observe some basic procedural steps,which may lead to technical difficulties but usually the situation is overcome by timely intervention or by modifying the technique.Here are some situations, where an anaesthesiologist may encounter difficulties during his routine anaesthesia practise when they fail to observe the basics.
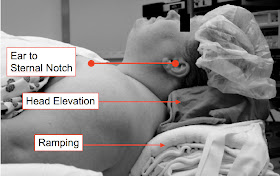
1)The importance of sniffing position with pillow under occiput:
The standard procedure for endotracheal intubation consists of keeping the head in sniffing position supported by pillow under head. Successful tracheal intubation is achieved by obtaining a good glottic
view,which requires alignment of three optical axes corresponding to the
oral, pharyngeal and laryngeal planes. Extension at the atlanto occipital joint together with a head elevation( moderate
head elevation 5–10 cm above the surgical table) keeps the perfect axis for an easy intubation[2]Infants may need a small towel roll under the "shoulders" to align the head.Obese patients [3]elevated head-up position or "ramp"position is used. In this position, the shoulders are elevated with several pads, the head and neck are extended, and the external auditory
meatus is in line with the sternal notch.Most the difficult airways arise due to defective positioning.
 figure 1
figure 1
figure 2
2)Bag and mask ventilation without oral airway and intubation without applying cricoid pressure.

One 9 year old boy with respiratory distress was admitted to A and E following ARDS due to severe sepsis.The child was conscious but drowsy and dropping saturation. The anaesthesiologist was called in for intubation and he continued with initial bag and mask ventilation to maintain the saturation while preparing for intubation.An airway was not used and the air pumped into his lungs negotiated its way to stomach due to partial airway obstruction. While he did laryngoscopy, due to gag reflex he regurgitated and immediately aspirated. Further attempts to maintain saturation following intubation were not successful. Drowsy semiconscious patients with weak gag reflex may tolerate oral airway and definitely tolerate nasal airway which helps to direct the air into the lungs following ambu bag ventilation.[4].The basic rule states application of cricoid pressure with head down position will prevent aspiration.(application of cricoid pressure and its effectiveness is questioned and many controversies exist, but was found very useful practically)

3)Intubation using a bougie in difficult airway.
Grades 2 and 3 glottic view may be managed by intubation over a bougie.Following laryngoscopy insert bougie into the glottis and then "rail road"the ETT over the bougie.The basic rule here is "dont remove the laryngoscope before railroading". Once you remove the scope after inserting bougie the epiglottis and pharyngeal soft tissues may come their way between the ETT and the bougie and cause intubation failure.Ask the assistant to pass the ETT over the bougie while the anaesthetist keeps the epiglottis elevated with his laryngoscope with one hand and stabilising the bougie with the other hand.

4)Removal of a Laryngeal mask airway.
Patients on spontaneous ventilation under LMA anaesthesia,it is advisable to remove the LMA in deep anaesthetic plane itself.If you wait till the patient is fully conscious,chance of biting the airway tube by patient is high which leads to total airway occlusion and any attempt to remove an LMA in this situation can cause damage to the LMA, laryngospasm or regurgitation by pharyngeal stimulation[5].The ideal sequence of removing LMA seems....remove in deep plane then cut down gases,insert oral or nasal airway,keep mask, turn head to one side, allow patient to recover by inhaling 100% oxygen.
5)Treating laryngospasm during recovery.
The treatment should be immediate,prompt and aggressive[6].Delay in treating laryngospasm may lead to serious morbidity.IPPV with 100% to break off the spasm is widely followed as the first line of management but there should not be any delay in administering suxamethonium.The most feared complications are hypoxia and negative pressure pulmonary edema.
6)Exsanguinate before IVRA.
Complete exsanguination of the upper limb is advocated before IVRA.Failure of proper exsanguination leads venous oozing during the procedure causing unsatisfactory operating conditions.Poor diffusion of the drug leads to 'patchy" anaesthesia or total failure of anaesthesia.The use of an esmarch or similar bandage is stressed.
7)Extubating a difficult airway.There are many gadgets available to deal with a difficult airway.With the introduction of fastrach LMA and fiberoptic bronchoscope, the success rate of intubation is high.Following ICU admission or surgical procedure many anaesthesiologists fail to observe the basic rule "while extubating a difficult airway take the same precaution and keep ready the same gadgets you used to intubate the case, since extubation failure or post extubation complications may necessitate immediate reintubation". Always use a guide wire or bougie over which the ETT is pulled out (extubation over bougie)and observe the vocal cord behaviour during extubation.
8)Testing loss of resistance. While testing for loss of resistance during epidural anaesthesia always use saline instead of air to avoid complications like pneumocephalus[7], spinal cord and nerve root compression, retroperitoneal air, subcutaneous emphysema, and venous air embolism[8] Alternatively saline with an air bubble technique also seems to be appropriate.
Performing the LOR by saline, from NYSORA9)Nasal intubation in pediatrics. Extreme caution should be taken while performing a nasal intubation in pediatric age group and any difficulty in ventilation should alert the anaesthetist of possibility of occlusion of the tip of ETT with a piece of adenoid tissue carried away in it. Any incidence of difficulty in ventilation, high airway pressure,abnormal tracing of capnogram or fall in saturation following nasal intubation in children,the anaesthetist should not hesitate to remove the ETT immediately and proceed with mask ventilation and oral intubation. Never attempt to overcome the resistance by forced ventilatory attempts or by passing catheters into ETT..[9][10]The obstruction by adenoid is usually distal to murphy's eye and other common causes for the obstruction are kinking of ETT and severe bronchospasm following intubation.
10)Uncover during PAC!The last but not the least, make a detailed physical examination during PAC.It was found on many occasions that gross physical deformities were overlooked by anaesthetists due to lack of proper exposure of body parts.Such deformities include pectus excavatum, pectus carinatum,scoliosis, thyroid swellings and other congenital abnormalities,.All these situations may lead to devastating intra operative complications.
Ref:
1)http://www.quotecounterquote.com/2010/12/to-err-is-human-to-forgive-divine.html
2)http://www.anesthesia-analgesia.org/content/early/2011/05/18/ANE.0b013e31821c7e9c.full.pdf
3)http://www.anesthesia-analgesia.org/content/102/5/1592.1.full
4)http://www.acep.org/Clinical---Practice-Management/Focus-On---Bag-Valve-Mask-Ventilation/
5)http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD007082/pdf
6) http://www.respond2articles.com/ANA/forums/thread/1096.aspx
7)https://www.aana.com/newsandjournal/Documents/p449-453.pdf
8)http://www.ncbi.nlm.nih.gov/pubmed/9010941
9)http://www.cas.ca/English/Page/Files/657_1344758.pdf
10)http://www.thefreelibrary.com/Nasotracheal+tube+occlusion+from+adenoid+trauma.-a0188739844