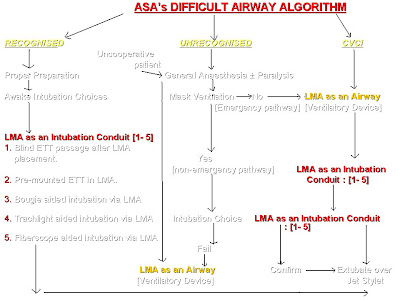
The recent development in the management of "difficult airway" is the incorporation of LMA into its algorithm. Since the introduction of LMA in 1981 they have been widely evaluated for their efficacy in managing difficult airways and have been proven effective in CICV situations.According to the 'Practice Guidelines for Management of the Difficult Airway' by the ASA task force, the use of supraglottic airway devices including LMA, Combitube or other suitable supraglottic airway as rescue devices in the “cannot intubate cannot ventilate” situation, is highly recommended. The advice switches from an earlier emphasis on laryngoscopy and intubation to an emphasis focusing on ventilation and oxygenation.The present topic concentrates only on the algorithm where LMA can be used as an intubation conduit. Eventhough intubating LMA is widely used to manage difficult airway, classic LMA alone is included in the algorithm because of its simplicity and safety in inexperienced hands. Watch the following flow charts, photographs, and a video which are self explanatory.
Classic LMA
- Developed by Dr. Archie I J Brain, a British anesthetist in 1981.
- First successful use of prototype LMA in failed intubation situation in a 114 kg patient in February 1983.
- Dr. Archie Brain publishes his first series of 23 patients undergoing routine airway management by the LMA in 1983.
- 21 cases of difficult intubations were managed by the LMA and reported in literature between 1983 - 1987.LMAs are commercially available since 1987.
- Simple to use
- Non-invasive design as it does not invade trachea
- An easy to learn & easy to teach quality.
- Improved success rate with minimal tissue trauma in first attempt
- Ability to be used as a ventilatory device as well as an aid to intubation.
- Immediate airway access compared to invasive techniques
- Less gastric inflation and subsequent regurgitation.

How to insert:
The standard technique:
Why and how LMA has found a unique place in Algorithm?
- Insert the deflated LMA with the laryngeal aperture facing cephalad and rotate it 180º as the cup enters the pharynx, Specially useful in patients with restricted mouth opening or hindrance to placement by tongue.
- Insert the LMA from the side of the mouth in emergency for example from bedside using thumb
- Insert the LMA with the cuff partially inflated when the deflated cuff gets folded.
- Insert the LMA with the aid of a laryngoscope again in difficult insertion due to large tongue, edentulous airway or due to restricted mouth opening.
- Insert LMA with the aid of stylet or a bougie as guide.
- In patients with a restricted mouth opening, LMA can be placed retro molar and subsequently the LMA tube is brought forward to lie centrally
ALGORITHM EXPLAINING THE ROLE OF LMA (EXPANDED)
Click on the image to enlarge
LMA AS AN INTUBATION CONDUIT:
- Blind passage of ETT through LMA: After placement of LMA by any one of the above techniques, the lubricated endotracheal tube is passed blindly through LMA and placement confirmed by auscultation, chest movement or by capnogram. The following table helps you to choose the correct size of ETT to be passed.
In an attempt to insert the LMA blindly one may encounter 2 levels of obstruction within the LMA.The first one is at the level of the aperture bar and the second one is at the level of glottic opening.
To overcome the first level of obstruction, the ETT is slightly bend and turned to one side while passing. The second level of obstruction is overcome by flexing the neck while insertion
- Premounted ETT in LMA with insertion:To avoid the problems associated with obstruction, the ETT is premounted on LMA and inserted. Subsequently manipulated to enter the glottis.
- Bougie aided intubation through LMA: The LMA is inserted cuff inflated and placement confirmed. A bougie is passed through the ETT and manipulated into the larynx. The LMA is deflated and removed and a lubricated ETT is passed over the bougie into the trachea
- Trachlight aided intubation via LMA: After placement of LMA a trachlight (lighted wand) is used to identify the laryngeal inlet and ETT is passed over it.
- Fiberoscope aided intubation via LMA: Similar to trach light, a fiberoptic bronchoscope is passed into the LMA to reach the trachea and subsequent intubation over bronchoscope is done.
When no aids are available in CVCI situation the algorithm advises on cricothyrotomy and transtracheal jet ventilation.An anteriorly placed larynx can be managed, in the absence of stylet or bougie by simple manipulation of the ETT, by anchoring it on middle finger to bring forward the tip of ETT.
The video and a few photographs are reproduced with permission from Dr.Rashid M Khan and Dr.Naresh Kaul of Khoula hospital Muscat, who conducted a workshop on "difficult airway" at ibri hospital in March 2010. The author is much thankful to them.
The video and a few photographs are reproduced with permission from Dr.Rashid M Khan and Dr.Naresh Kaul of Khoula hospital Muscat, who conducted a workshop on "difficult airway" at ibri hospital in March 2010. The author is much thankful to them.
Ref:1)ASA, Practice guidelines for the management of difficult airway -2003 . www.asahq.org/publicationsAndServices/Difficult%20Airway.pdf
2)Leader GL, facilitation of insertion of Laryngeal mask, Anaesthesia 1991;46:987
3)The Difficult Airway in Adult Critical Care.: Supraglottic Airway ,www.medscape.com
2)Leader GL, facilitation of insertion of Laryngeal mask, Anaesthesia 1991;46:987
3)The Difficult Airway in Adult Critical Care.: Supraglottic Airway ,www.medscape.com