More than pain, he was worried of the disfigurement it caused.A small nevus just above the right eyebrow was a source of worry and disappointment which made him think of a cosmetic repair for better appearance. Mathew Davids,a 38 year old software engineer from India and employed in USA flew to his home country eventhough one of the US hospitals (with the best facil ities in world) offered a cosmetic cum plastic repair for him within affordable cost.He thought he will be more comfortable amidst of friends and relatives.
More than pain, he was worried of the disfigurement it caused.A small nevus just above the right eyebrow was a source of worry and disappointment which made him think of a cosmetic repair for better appearance. Mathew Davids,a 38 year old software engineer from India and employed in USA flew to his home country eventhough one of the US hospitals (with the best facil ities in world) offered a cosmetic cum plastic repair for him within affordable cost.He thought he will be more comfortable amidst of friends and relatives.After 2 days he was scheduled for surgery. The pre anaesthetic check went smooth except for an elevated diastolic BP record of 94 mmHg. He was given GA spontaneous following propofol induction and fentanyl infusion using classic LMA. Maintenance of anaesthesia was with 4-6% sevoflurane in oxygen and nitrous oxide.Intra operative BP, SPO2, ETCO2 and HR were within normal limits. Surgery completed in 32 minutes, LMA removed and he was shifted to recovery room.He was drowsy but arousable.
The recovery nurse who was busy with the management of some major post operative cases thought that his surgery is too short and doesn't require intensive monitoring.The oxygen mask was applied to his face but the other end of the tubing got disconnected on patient movement and was un noticed
There is a fall in saturation and SPO2 low alarm on monitor alerted the staff nurse. She rushed to his trolley and found him unresponsive and cyanosed.The monitor showed severe bradycardia and ST elevation on ECG. Immediate mask ventilation, CPCR and intubation followed.Patient was shifted to ICU where a 12 lead ECG showed STEMI and the troponin value was raised.A decision to thrombolyse was made and initiated. He was on ventilator for three days and got discharged without any neurological deficit.The probable cause for this incidence was thought to be diffusion hypoxia with hypercarbia.Who is the cul prit here? The anaesthesiologist who kept the patient in deep inhalational plane maintaining spontaneous ventilation for 32 minutes or the recovery nurse who neglected the importance of administering oxygen for a GA case?
Diffusion hypoxia (fink effect) means outpouring of large volumes of nitrous oxide into the lung during recovery from general anaesthesia and subsequent hypoxia.This is due to
1) Direct replacement of oxygen from lung
2) Diluting alveolar carbon dioxide causing decreased drive for ventilation.
This effect is seen in first 5-10 minutes of recovery when large volumes of nitrous oxide is released into the lung.The blood gas solubility of nitrous oxide is 0.42 which is less than that of any other inhalational agents.So rapid alveolar concentration following inhalation.But N2O is more soluble than nitrogen in blood. Hence blood and body fluids are rich in N2O.At the end of anaesthesia N2O diffuses back into alveoli from blood down a concentration gradient and this diffusion back is rapid than uptake of nitrogen from the alveoli by blood. This leads to replacement of all alveolar gases by nitrous oxide and subsequent hypoxia.
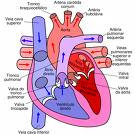
Fig. showing relationship between O2 and N2O following recovery.
So it is mandatory that 100% oxygen should be given for all GA cases following recovery for about 5-10 minutes to avoid the occurrence of diffusion hypoxia
Ref: 1) Millers Anaesthesiology 7th edition
2John L.Bezzant,M.D, http://library.med.utah.edu/kw/derm/nitrous/05ni.htm