A 7 year old boy is presented with chest discomfort and palpitation. He is also complaining of right iliac fossa pain.The pulse rate is 174/mt, BP 94/50 with mild elevated JVP. The monitor showed supraventricular tachycardia which responded to carotid sinus massage. He is febrile and has pallor.Chest is clear and CVS examination revealed an ejection systolic murmur of grade 2/4 radiated along left parasternal border and tachycardia. Abdominal examination showed Rt. iliac fossa tenderness with guarding.Lab findings were normal except for a high WBC count and Hb value of 9 Gms%. Previous records showed one ER admission with palpitation and the diagnosis was marked as suspected Cardiomyopathy(unclassified) with a probable viral etiology.The monitor again showed rapid pulse rate and the ECG is characteristic of supraventricular tachycardia with no response to carotid sinus massage this time.The patient was shifted to ICU for stabilisation, Oxygen by mask applied and cardiovascular status monitored. Inj. adenosine was given 2.6 mg iv and the heart rate slowed down initially to 100/mt but raising,so an immediate second bolus of adenosine 5.2 mg was given.Controlled fluid management started and temperature was maintained.The heart rate reduced to 132/mt and a second ECG showed SVT with QRS duration of .08 with QT 0.45 secs
The HGT was 5.5 and ABG showed mild respiratory alkalosis.Abdominal examination revealed acute appendicitis and was confirmed by ultrasonography.A decision to operate was made.The patient was administered amiodarone 5mg/kg and infusion 2.5 mic/kg/mt followed.The CXR showed cardiomegaly and an echocardiogram showed dilated left ventricle with global hypokinesia and impaired systolic function, posteriorly displaced mitral valve with MR, ejection fraction of 40%, all suggestive of a dilated cardiomyopathy.The heart rate is now stabilised on amiodarone and the cardiologist was consulted for the management of any intraoperative adverse events and to prepare for a temporary pacemaker insertion as an emergency intervention.Aspiration prophylaxis was given, Midazolam 1mg was given IV and the patient was shifted to operation theatre.
ECG, Oxygen saturation,Temperature ,NIBP etc were monitored. Anaesthesia was induced with IV ketamine 1 mg/kg and propofol 1mg/kg, along with IV fentanyl 1mcg/kg supplemented with oxygen, nitrous oxide and 1-1.5% isoflurane.Vecuronium was used to facilitate intubation at the dose of 1.5 mg/kg.(1) The heart rate and BP were stable throughout the procedure and a baseline infusion of amiodarone 1-2mic/kg/mt was on flow.Anaesthesia was maintained with O2/N2O in isoflurane (MAC 1-1.5) and intermittent boluses of vecuronium bromide IV, An arterial line and central venous catheter were inserted.TEE was not available. An esophageal stethescope was introduced. The capnogram waveforms are carefully observed.A central venous pressure of 6-8 cm of H2O was maintained by controlled fluid administration. Ideally a pulmonary artery catheter is indicated to monitor the filling pressures along with TEE. The reversal of neuromuscular block was achieved with neostigmine and glycopyrrolate and the postoperative period was uneventful.The child is stabilised on amiodarone 125 mg bid dose and was discharged with a maintenance dose of atenolol 25 mg so as to prevent the long term complications of amiodarone like thyroid dysfunction and pulmonary toxicity.
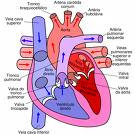
Dilated cardiomyopathy is characterised by left ventricular or biventricular dilatation and impaired ventricular contractility.The most common complication of dilated cardiomyopathy is progressive congestive cardiac failure.The commonest etiology is idiopathic or viral infections in children and alcohol abuse in adults.Most of the patients are asymptomatic with cardiomegaly and minimal CVS symptoms and present later in the course with cardiac failure, when the mortlity rate is high.The predictors of poor prognosis are(2) an ejection fraction of less than 0.25 (as seen on Echo, during the acute presentation of heart failure), left ventricular end diastolic dilatation, a hypokinetic left ventricle, the presence of mitral and tricuspid regurgitation
The goals (3) of anaesthetic management are
- Myocardial depression should be avoided
- Normovolemia is maintained
- To avoid overdose of drugs during induction as the circulation time is slow.
- Ventricular afterload is avoided
- Avoid sudden hypotension when regional anaesthesia is the choice
- Induction by midazolam/nitrous oxide/ vecuronium /isoflurane for GA
- Graded epidural anaesthesia with sedation using midazolam.The advantages are adequate post operative analgesia and less hemodynamic alteration.The changes in preload and afterload produced by epidural anesthesia mimic the pharmacological goals of treatment.(3) Here an anaesthetic level upto T4 is required and a well relaxed abdominal muscles are preferred.To achieve this goal the dosage of local anaesthetic requirement would be high which may precipitate sudden change in hemodynamics and the treatment of hypotension with ephedrine further worsens the CVS status.Phenylephrine if used to treat hypotension may cause increase in afterload which is detrimental.Hence the decision to administer GA.
1)Yamaguchi S, Wake K, Mishio M, et al. Anesthetic management of a patient with dilated cardiomyopathy under total intravenous venous anaesthesia with propofol and ketamine combined with continuous epidural analgesia. Masui 1999;48: 1232-34.
http://www.ncbi.nlm.nih.gov/pubmed/10586558
2 WILLIAM G, VALENTIN FUSTER: Idiopathic dilated Cardiomyopathy. New England Journal of Medicine; 331:1564-75, 1994.
3. ROBERT STOELTING K, STEPHEN F: Anesthesia And Co-Existing Disease, 4th Edition Lippincott-Raven; Ch. 7:117-120.

No comments:
Post a Comment
PLEASE LEAVE YOUR COMMENTS BEFORE YOU LEAVE